Patient’s Guide to Living with Glaucoma
Discovering the Sneak Thief: Diagnosing Glaucoma
Because it often goes undetected in its early stages, glaucoma is called the “sneak thief of sight.” It is estimated that nearly half of the Americans who currently have glaucoma are unaware of their condition. The reasons that glaucoma so often goes undetected include the following:- Most types of glaucoma are painless, with no feelings of discomfort.
- There are rarely noticeable visual symptoms early on in the disease; early vision loss occurs at the peripheral areas of vision.
- Glaucoma often affects one eye with more severity than the other, and our binocular visual systems are effective at compensating for defects in one eye.
- Changes to vision caused by glaucomatous damage are usually quite slow; it can be difficult to notice gradual changes.
- Most vision screening programs are relatively short examinations aimed at identifying the presence of a vision problem or a potential vision problem, and are not designed to screen specifically for glaucoma. (See The Difference between a Vision Screening and a Comprehensive Eye Examination and How Can I Detect Glaucoma if There Are No Initial Symptoms?)
- Glaucoma tests often rely on elevated eye pressure as the primary or sole indicator of the disease; recent research suggests that the dilated eye exam may be a more accurate method for detection of glaucoma.
- Glaucoma is often associated with aging, and subtle changes to vision are often accepted as part of “getting older.”
- Many people are unaware of their own risks for glaucoma and the critical importance of preventive eye care.
- For many people, professional eye care is difficult to obtain or beyond their financial reach.
What is Glaucoma?
Glaucoma is a term applied to a group of conditions that all lead to progressive optic nerve damage (neuropathy). This nerve damage affects the visual system by damaging and ultimately killing the retinal ganglion cells that transmit visual information from the retina to the brain. Although glaucoma may not be considered solely as an “eye disease,” the bottom line is damage to or degeneration of the optic nerve. Glaucoma is characterized by:- a specific pattern of optic nerve head damage called “cupping”
- an identifiable pattern of visual field loss
Getting Checked Out
Glaucoma can be discovered in the course of a comprehensive dilated eye examination. Regular eye exams are the key to detecting glaucoma early enough for effective treatment.- Professional ophthalmology guidelines now recommend comprehensive eye examinations every three to five years, beginning at least by age 40. If you have risk factors for glaucoma, you should have your first comprehensive eye exam before age 40.
- If you have glaucoma risk factors or are 65 years old or older, the American Academy of Ophthalmology (AAO) recommends an exam or screening every two years.
- If you are of African, Hispanic, or Asian descent, your doctor may well recommend regular eye exams starting in your 20s or 30s, as studies indicate that you may have a higher risk of developing glaucoma.
Finding the Right Eye Doctor
The eye doctor performing your examination should be experienced in the diagnosis of glaucoma, and you should be comfortable with her style and approach. Ask your doctor if she will be performing glaucoma-specific tests and examinations.Questions for Your Doctor
- Which glaucoma tests should I have?
- What do these tests involve?
- Do you have the equipment needed to perform these tests? If not, where will the tests be carried out?
- Will the tests hurt?
- How often should I be tested for glaucoma?
- How long will it take to learn the results?
- What do I need to do to in order to find out the test results?
Test Results and Diagnosis
Glaucoma is usually diagnosed when examination and/or testing shows one or both of the following:- Structural changes: characteristic optic nerve head and the retinal nerve fiber layer degeneration.
- Loss of functional vision: defects in visual fields that match the structural changes.
- You do not have glaucoma and are not currently at risk for developing glaucoma.
- You do not appear to have glaucoma but you have risk factors that indicate that further examination by an ophthalmologist is in order, or that you should return for periodic re-examinations.
- You have glaucoma.
Glaucoma Tests
There is no single test for determining whether you have glaucoma or are at risk of developing glaucoma. The clinician examining you must interpret your medical history (including any earlier examination findings), family history (genetics), and results from clinical observation of your optic nerve head and diagnostic test(s), and then assess if 1) there are structural changes and/or loss of functional vision that require treatment, or 2) if you are at risk of such damage and should begin treatment to manage potential disease. To detect glaucoma you should have a comprehensive dilated eye examination with an emphasis on these assessments:- Ophthalmoscopy: examines the optic nerve
- Tonometry: measures intraocular pressure (IOP)
- Pachymetry: measures corneal thickness
- Perimetry: measures visual fields
- Gonioscopy: assesses the anatomical angle formed between the cornea and iris
Examining the Optic Nerve: Ophthalmoscopy
The examination of the optic nerve head and retinal nerve fiber layer for signs of glaucomatous damage is a critical part of detecting and diagnosing glaucoma. There are three types of ophthalmoscopy examination: direct, indirect, and slit-lamp. The two most common are slit-lamp ophthalmoscopy and direct ophthalmoscopy. With both of these methods, to provide a better view of the back of your eyes, your pupils will be dilated (enlarged) with drops that will make your eyes more sensitive than normal to light for several hours. The drops dilate the pupil either by contracting the muscles that enlarge the pupil or by relaxing the muscles that make the pupil constrict and the muscles that focus the lens of the eye. These most common forms of ophthalmoscopy exam are not uncomfortable or painful, although the very bright examining light may distort your vision for a few minutes. You may experience light sensitivity and blurred vision for a short time after having your eyes dilated. The blurred vision will make it more difficult to read up close. Distance vision is normally not significantly affected by dilation.Slit-lamp Ophthalmoscopy
Consisting of a low-power microscope combined with a high-intensity light beam, and often with the help of a dye applied to the eye, the slit-lamp exam is used to examine the structures at the front of the eye: eyelids, cornea, conjunctiva, sclera, iris, and the tear layer. Caption: Slit-lamp examination. Source: NEI/NIH
During a slit-lamp exam, a microscope and a small lens are placed close to the front of your eye while you sit with your chin and forehead on a support to keep your head steady.
Caption: Slit-lamp examination. Source: NEI/NIH
During a slit-lamp exam, a microscope and a small lens are placed close to the front of your eye while you sit with your chin and forehead on a support to keep your head steady.
Direct Ophthalmoscopy
With the room darkened, the examiner shines a beam of light from the direct ophthalmoscope through the pupil and views the back of the eye with a variety of lenses.Visualizing and Assessing the Optic Nerve Head
When performing an ophthalmoscopy, your doctor will be looking for indications of structural loss of retinal ganglion cells and their fibers.Cup-to-disc Ratio
The cup-to-disc ratio is an important measurement. Glaucoma causes the fibers of the ganglion cells that form the rim of the nerve head to die. As a result of this cell death, the central cup—the space in the middle of the nerve head left behind when nerve cells die—gets larger and the rim of healthy nerve fibers gets smaller.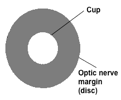 Caption: A graphic representation of the cup and disc of the optic nerve head. Source: Author.
Caption: A graphic representation of the cup and disc of the optic nerve head. Source: Author.
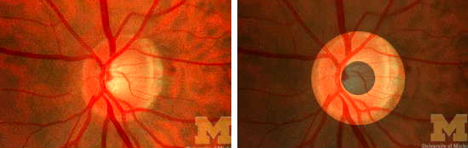 Caption: The normal optic disc is shaped like a donut. Source: University of Michigan College Eye Center.
As glaucoma progresses, the cup-to-disc ratio increases. The average cup-to-disc ratio of a healthy eye is 0.3–0.4. A cup-to-disc ratio of 0.7 or higher is considered an indication of glaucoma.
Because early glaucoma typically affects one eye more than the other, a big difference between the cup-to-disc ratios of the two eyes—asymmetry—is another sign of glaucoma.
Caption: The normal optic disc is shaped like a donut. Source: University of Michigan College Eye Center.
As glaucoma progresses, the cup-to-disc ratio increases. The average cup-to-disc ratio of a healthy eye is 0.3–0.4. A cup-to-disc ratio of 0.7 or higher is considered an indication of glaucoma.
Because early glaucoma typically affects one eye more than the other, a big difference between the cup-to-disc ratios of the two eyes—asymmetry—is another sign of glaucoma.
Thickness of the Neuroretinal Rim
Your examiner will also be looking for patterns of thickness and areas of thinning of the neuroretinal rim—the area of the optic disc that contains the ganglion cell—and for signs of glaucomatous process.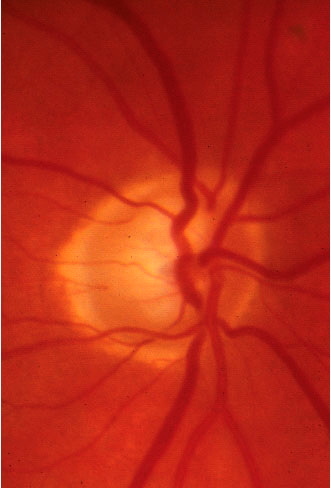 Caption: An optic disc with neuroretinal rim thinning. Source: University of Michigan College of Optometry.
Caption: An optic disc with neuroretinal rim thinning. Source: University of Michigan College of Optometry.
Notching
Notching, or loss of fibers in one area of the rim of the optic nerve head, can indicate glaucoma in eyes that may not yet have a large cup-to-disc ratio.Bleeding
Visible signs of bleeding on the nerve head in the form of small splinter-like hemorrhages rarely occur in non-glaucomatous eyes. Although these hemorrhages are easily overlooked during exam, they are a good indication that glaucoma is present. Although hemorrhaging usually disappears, it often leaves behind notching of the rim.Thinning of the Retinal Nerve Fiber Layer
In addition to the nerve head, the examiner should observe the state of your retinal nerve fibers (RNFs). Lost RNFs are an indication of glaucoma and an early predictor of functional glaucoma damage.Optic Nerve Imaging
Photographing the optic nerve head allows a doctor to assess change over time to determine whether glaucoma is progressing. Stereoscopic photography, the current gold standard for assessing optic nerve change, is now being used in conjunction with digital imaging that not only records the optic nerve head and nerve fibers but also measures and quantifies structural changes of nerve fiber thickness. Several imaging systems now provide quantitative measures of the optic nerve head and retinal nerve fiber layer. While these new imaging technologies can precisely quantify structural measurements of the optic nerve head and retinal nerve fiber layer, they do not replace physical inspection of the optic disc, other tests, or the evaluation of risk factors. They do provide important quantifiable data to be integrated with the other information gathered in examination.Limitations of Assessing the Optic Nerve Head
If all optic nerve heads looked the same, ophthalmoscopy would accurately identify glaucoma nearly 100 percent of the time. But the structure of optic nerves varies from person to person, which can make diagnosis challenging. Visual assessment of the optic nerve is a subjective process. Standardized methods for analyzing and measuring glaucomatous disc damage have been proposed, but for now these systems are still considered time-consuming and impractical to use.After Your Ophthalmoscopy
After your ophthalmoscopy, your doctor may or may not tell you what he found. If he doesn’t, ask! Find out your cup-to-disc ratio. Ask if the doctor found any nerve fiber loss. If pictures were taken, ask to see them and to have them explained.Measuring Intraocular Pressure: Tonometry
Tonometry, the measurement of intraocular pressure (IOP), has been a cornerstone of glaucoma evaluation for many years. In fact, testing IOP was long considered testing for glaucoma.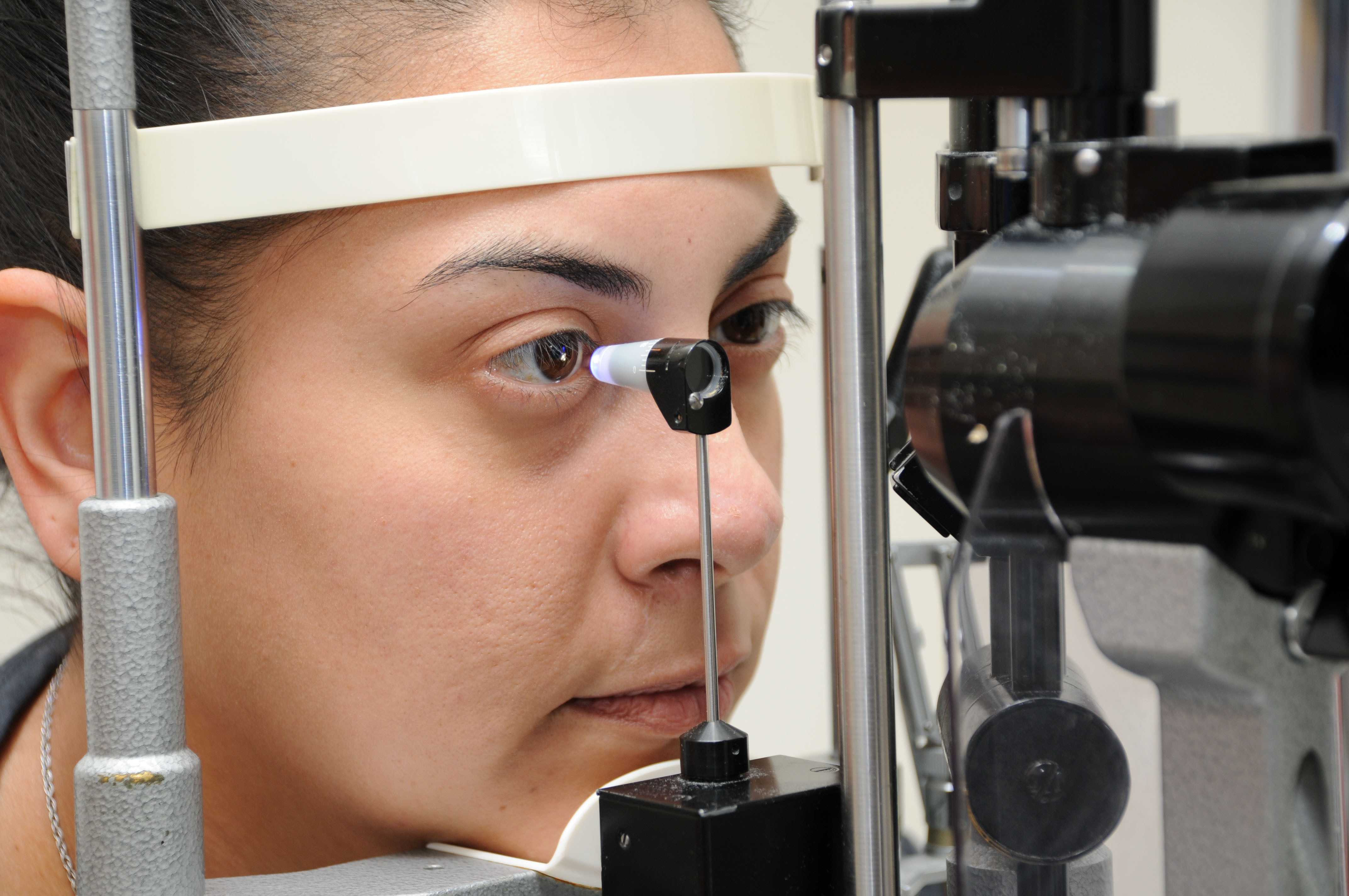 Caption: Testing IOP with a Goldmann tonometer. Source: Courtesy Karanjit Kooner MD and William Anderson, photographer, University of Texas Southwestern Medical Center, Dallas.
Pressure is still an essential component of glaucoma screening because of the known association between elevated IOP and glaucoma. The most common tonometry methods measure the force required to flatten an area of the cornea.
Caption: Testing IOP with a Goldmann tonometer. Source: Courtesy Karanjit Kooner MD and William Anderson, photographer, University of Texas Southwestern Medical Center, Dallas.
Pressure is still an essential component of glaucoma screening because of the known association between elevated IOP and glaucoma. The most common tonometry methods measure the force required to flatten an area of the cornea.
The Goldmann Tonometer Exam
You may have had your pressure checked in the past with a tonometer that uses a puff of air to flatten the cornea. The Goldmann tonometer, which uses physical pressure instead of air to take the measurement, is now considered the gold standard and is preferred over the air-puff tonometer, which has been found in tests to significantly underestimate IOP measurement in eyes with elevated IOP. The Goldmann tonometer is accurate to within 1 to 2 mm Hg. (Pressure is measured in terms of millimeters of mercury or mm Hg.) The Goldman tonometer measures IOP by pressing against a small area of your cornea and measuring the force required to applanate (flatten) that area. You will receive a few numbing drops before the test. While the test is painless and requires no action on your part, certain conditions can affect your IOP reading. For an accurate reading, take a few calming breaths before resting your chin and forehead on the tonometer. Breathe normally. Do not hold your breath, as this may result in an IOP reading higher than your actual pressure. Very tight fitting collars, scarves, and the like can also artificially raise your IOP.Other IOP Tests
 Caption: Tono-Pen Applanation Tonometer. Source: Courtesy Karanjit Kooner MD and William Anderson, photographer, University of Texas Southwestern Medical Center, Dallas.
Portable, hand-held instruments for testing pressure such as the Tono-Pen and Perkins tonometer may be used in temporary screening clinics.
Caption: Tono-Pen Applanation Tonometer. Source: Courtesy Karanjit Kooner MD and William Anderson, photographer, University of Texas Southwestern Medical Center, Dallas.
Portable, hand-held instruments for testing pressure such as the Tono-Pen and Perkins tonometer may be used in temporary screening clinics.
IOP Fluctuations and Home Monitoring
Intraocular pressure is known to fluctuate from day to day as well as throughout the day. Yet a single reading during an ophthalmology appointment may be a major factor in a treatment plan that may include expensive medications and even surgery. One potential solution to the need to observe your IOP more frequently than your visits to the doctor is the do-it-yourself tonometer. Having an easy-to-use small tonometer allows you to test your pressures throughout the day as well as from day to day. At this point in time these devices are quite expensive. However, observing daily variation can be an important factor to report to your doctor. (See the FitEyes website for an ongoing discussion of home monitoring IOP.)After your Tonometry Exam
If the examiner doesn’t tell you your pressure as they measure it, ask!Measuring Corneal Thickness: Pachymetry
The thickness of the cornea can affect the IOP reading.- Thicker than normal corneas can result in IOP readings that are inaccurately high.
- Thin corneas can result in IOP readings that are inaccurately low.
Thinning Corneas: A Risk Factor for Glaucoma
In addition to their role in underestimating IOP, thinning corneas are now thought to be a risk factor for glaucoma. In the Ocular Hypertension Treatment Study those with the highest IOP levels and the thinnest corneas had the highest risk of glaucoma after five years.The Pachymetry Exam
After you receive an anesthetic eye drop, your corneal thickness is measured by gently touching the smooth tip of the pachymeter probe to the surface of the cornea. The probe emits a painless ultrasound wave that measures the corneal thickness. Caption: Measuring corneal thickness with a pachymeter. Source: Accutome.
Caption: Measuring corneal thickness with a pachymeter. Source: Accutome.
Mapping the Visual Fields: Perimetry
While optic nerve examination seeks to uncover structural damage to the optic disc and/or RNFs, perimetry maps your field of vision and shows where and how much vision has been lost. You might think that surely you would notice if you’ve lost some functional vision, but your eyes and brain are good at making up for gaps in vision. This is especially true of peripheral vision, the vision that glaucoma usually affects first. Perimetry provides a visual map and quantified evaluation of your vision.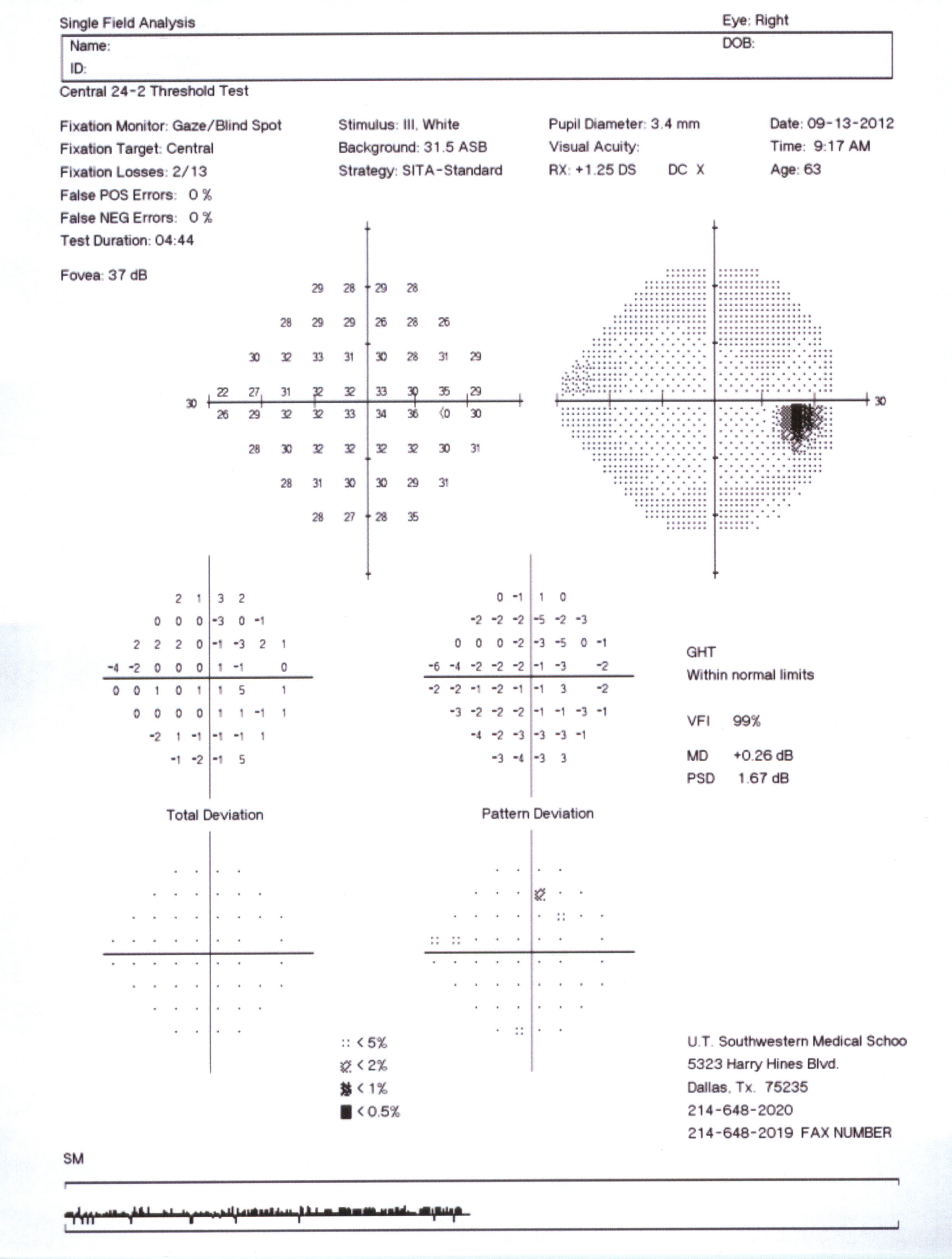 Caption: Map of a normal visual field. Source: Courtesy Karanjit Kooner MD and William Anderson, photographer, University of Texas Southwestern Medical Center, Dallas.
Because visual field tests take some time to complete and require the attention of a technician, they are often not given as part of a comprehensive eye exam unless there is a suspicion of glaucoma such as a high IOP measurement or observable changes to the optic nerve disc.
Caption: Map of a normal visual field. Source: Courtesy Karanjit Kooner MD and William Anderson, photographer, University of Texas Southwestern Medical Center, Dallas.
Because visual field tests take some time to complete and require the attention of a technician, they are often not given as part of a comprehensive eye exam unless there is a suspicion of glaucoma such as a high IOP measurement or observable changes to the optic nerve disc.
The Humphrey Field Analyzer
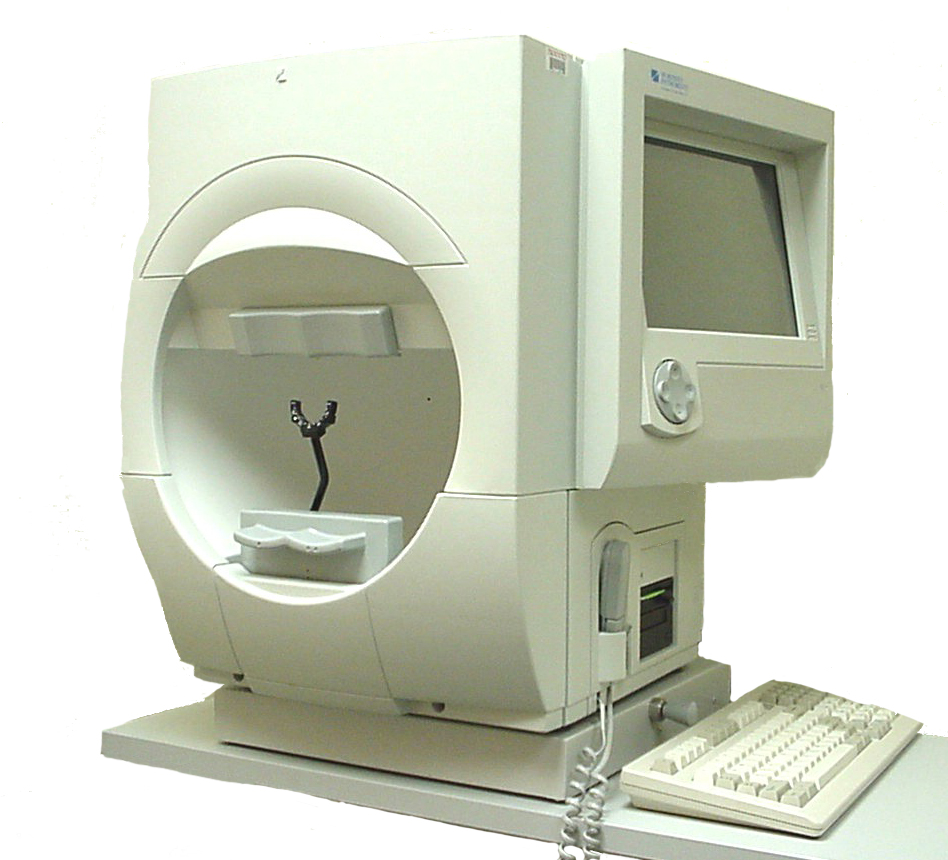 Caption: Humphrey Field Analyzer. Source: Courtesy Karanjit Kooner MD and William Anderson, photographer, University of Texas Southwestern Medical Center, Dallas.
The most commonly used visual field machine for perimetry, the Humphrey Field Analyzer, looks much like a large concave bowl. With one eye covered with a patch, you focus your vision on a central spot while small white lights of varying brightness flash at various points around the bowl. When you see a flashing light, you press a button. The test records which lights you see and which you do not, and in this way it creates a map of your visual field.
Caption: Humphrey Field Analyzer. Source: Courtesy Karanjit Kooner MD and William Anderson, photographer, University of Texas Southwestern Medical Center, Dallas.
The most commonly used visual field machine for perimetry, the Humphrey Field Analyzer, looks much like a large concave bowl. With one eye covered with a patch, you focus your vision on a central spot while small white lights of varying brightness flash at various points around the bowl. When you see a flashing light, you press a button. The test records which lights you see and which you do not, and in this way it creates a map of your visual field.
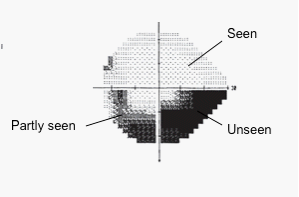 Caption: Map of visual field deficits. Source: Author.
Caption: Map of visual field deficits. Source: Author.
The Perimetry Exam with a Humphrey Field Analyzer
Visual field tests can be challenging at first. Keeping your focus on the central spot can be quite difficult. The instinctive response to a blinking light is to move your eyes to focus directly on it, but doing so in a field test would not show where your peripheral vision may be lost or compromised. The machine indicates when your focus has shifted, and the operator will remind you to focus on the central point. Another challenging aspect of the field test can be the amount of time during which you do not see anything to respond to. The flashing lights not only move around; they also vary in intensity. The test seeks to find the brightness threshold below which you cannot see at various points around your visual field, so there will be several periods of time during the test where you will not see anything at all. For those with significant visual field loss, this aspect of the test can be frustrating. If you have lost vision in areas of your visual field, you will not see anything to respond to when lights flash in those areas. Without regular stimulus to respond to, it’s easy to lose mental focus (and even fall asleep). There is also a learning curve involved with field tests. As you do more and more of them you will most likely become more comfortable with the process. Your doctor will hopefully repeat field tests to verify findings.Perimetry Tips
- Don’t start the test until you are comfortably seated, positioned at a comfortable height with your head resting comfortably in the headrest. A minor discomfort at the beginning can intensify into a distraction that takes your attention away from the test.
- The room should be dark. Lighting will affect your ability to see the targets; discuss lighting conditions with the technician.
- Remember, you are not trying to pass a test, nor can you fail. Do not try to beat the system by pressing the button when you’re not sure if you saw something. Remember that the system is designed to present stimuli you can’t see—that’s how it determines your threshold vision. Accumulating “false positives” by clicking when you are unsure if you have seen a light can result in an inaccurate assessment of the amount and severity of visual field loss.
- If there are distractions in the room, inform the technician.
- Try to avoid taking the test when you are sleepy or fatigued.
- Blink normally throughout the test.
- If you feel you need to stop and take a break, do so. Holding down the response button will pause the test, or you can ask the technician to pause the test.
After your Perimetry Exam
If your doctor does not show you your field test results, ask to see them. Not only will these results be used in treatment decisions, but also the tests evaluate where in your visual field you don’t see well any more, information that is invaluable to you in your daily life.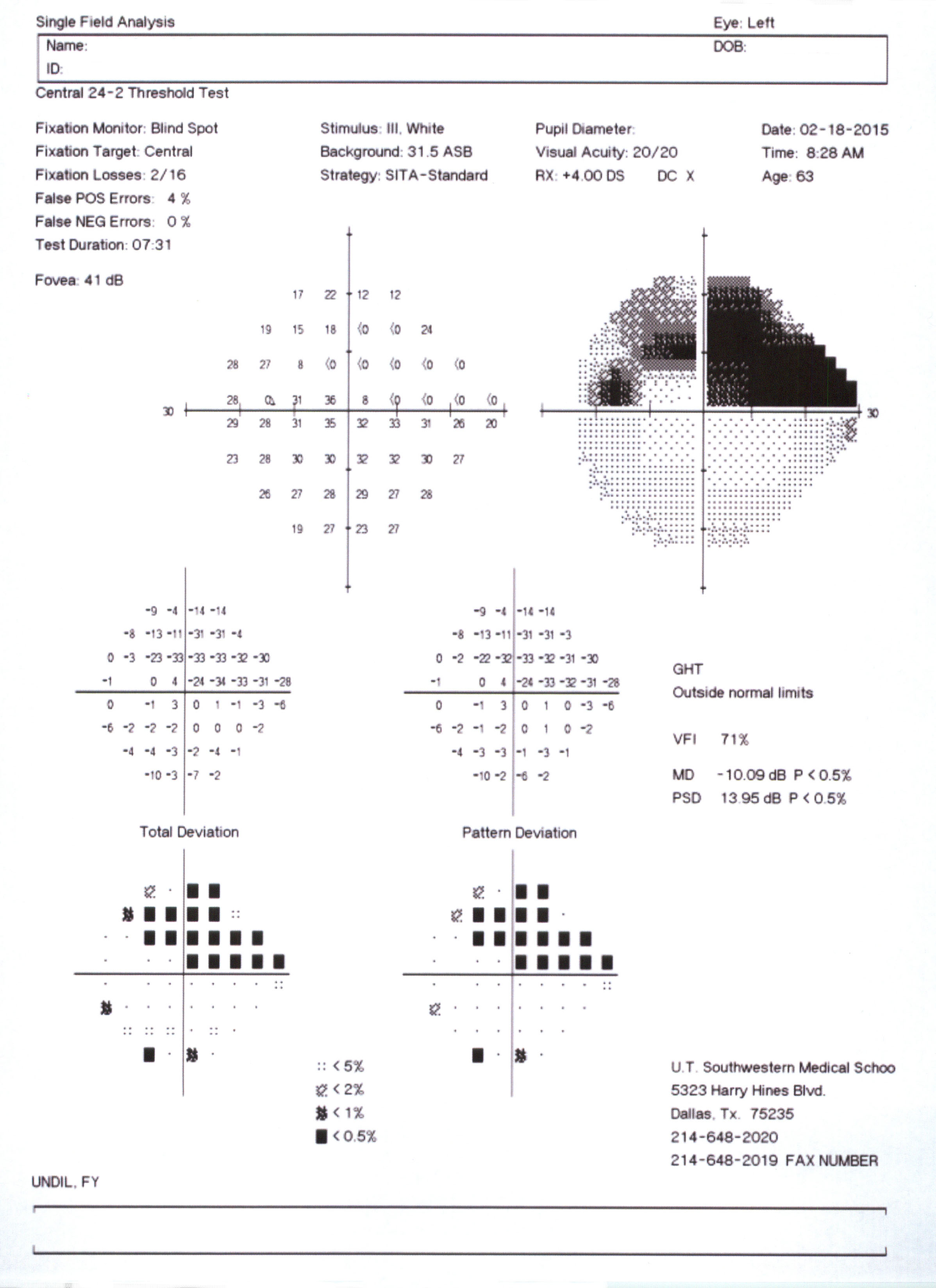 Caption: Visual field map showing moderate visual field damage. Source: Courtesy Karanjit Kooner MD and William Anderson, photographer, University of Texas Southwestern Medical Center, Dallas.
Caption: Visual field map showing moderate visual field damage. Source: Courtesy Karanjit Kooner MD and William Anderson, photographer, University of Texas Southwestern Medical Center, Dallas.
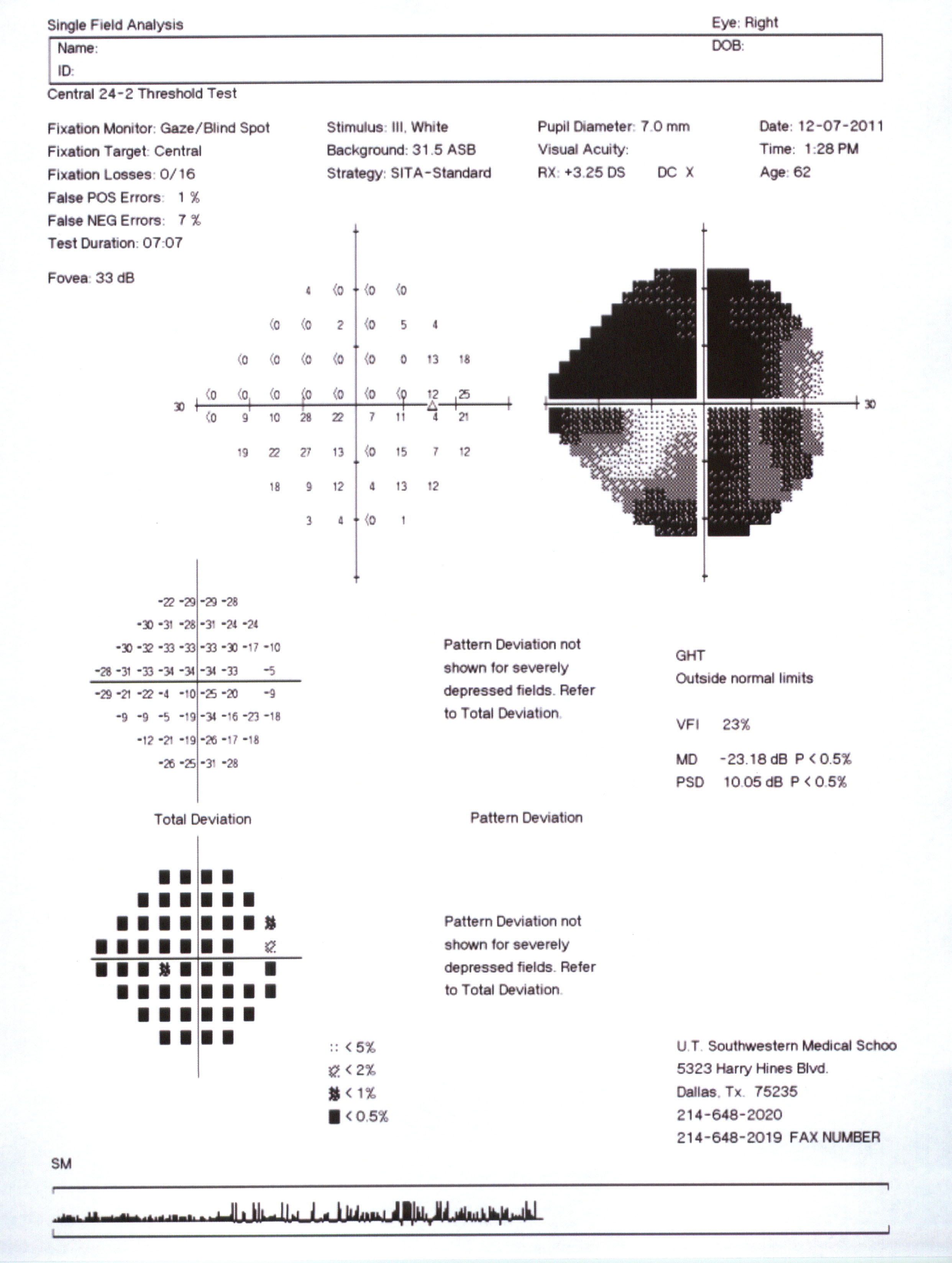 Caption: Visual field map showing advanced visual field damage. Source: Courtesy Karanjit Kooner MD and William Anderson, photographer, University of Texas Southwestern Medical Center, Dallas.
The printout of your visual field test shows both graphically and numerically the extent of any glaucomatous deficit you may have. The sensitivity of each point in the visual field is measured on a scale of 0–30 decibel units. These sensitivity measurements are graphically represented with darker areas indicating loss of sensitivity: the darker the shading, the more vision has been lost.
Caption: Visual field map showing advanced visual field damage. Source: Courtesy Karanjit Kooner MD and William Anderson, photographer, University of Texas Southwestern Medical Center, Dallas.
The printout of your visual field test shows both graphically and numerically the extent of any glaucomatous deficit you may have. The sensitivity of each point in the visual field is measured on a scale of 0–30 decibel units. These sensitivity measurements are graphically represented with darker areas indicating loss of sensitivity: the darker the shading, the more vision has been lost.
Central Vision Testing
Glaucoma is often so strongly associated with peripheral vision loss that central vision loss due to glaucoma can be overlooked. Paracentral scotomas—blind spots adjacent to the macula or central region—are in fact one of the identifiable patterns of visual field loss associated with glaucoma. Because clinicians often focus on blind spots in the periphery, a glaucoma patient’s loss of contrast sensitivity (the ability to detect differences between light and dark areas) or difficulty reading are often overlooked, even though these losses may affect the patient’s life (leading to falls and broken bones, for example). Clinicians managing glaucoma today often focus their testing on peripheral fields, performing 24-degree field tests, which assess peripheral vision loss, but choosing not to offer 10-degree visual field tests, which assess central vision. Ask for a central visual field test if your doctor does not include one in your exam.Other Perimetry Tests
Because standard automated perimetry tests such as the Humphrey do not identify visual field defects until significant numbers of ganglion cells have been lost, alternative tests that can identify glaucomatous damage earlier in the disease process are being developed and implemented.Examining the Angle: Gonioscopy
Because angle-closure glaucoma requires immediate medical attention, it is important to examine the drainage canals, or angles, for both eyes to ensure that they are functioning properly. Because the drainage angle for the eye is located around a “corner” of the cornea, the examiner can’t see whether your angle is open by looking directly in the eye. Gonioscopy uses a lens with a mirror to view the angle and determine two things:- Is the angle open or closed?
- Has the iris become stuck to the trabecular meshwork (an area of tissue responsible for draining)? This may indicate past, significant angle closure.
The Gonioscopy Exam
During the exam, the gonioscope is placed directly on the surface of your eye like a big contact lens. The examiner uses a slit-lamp biomicroscope to view the angle.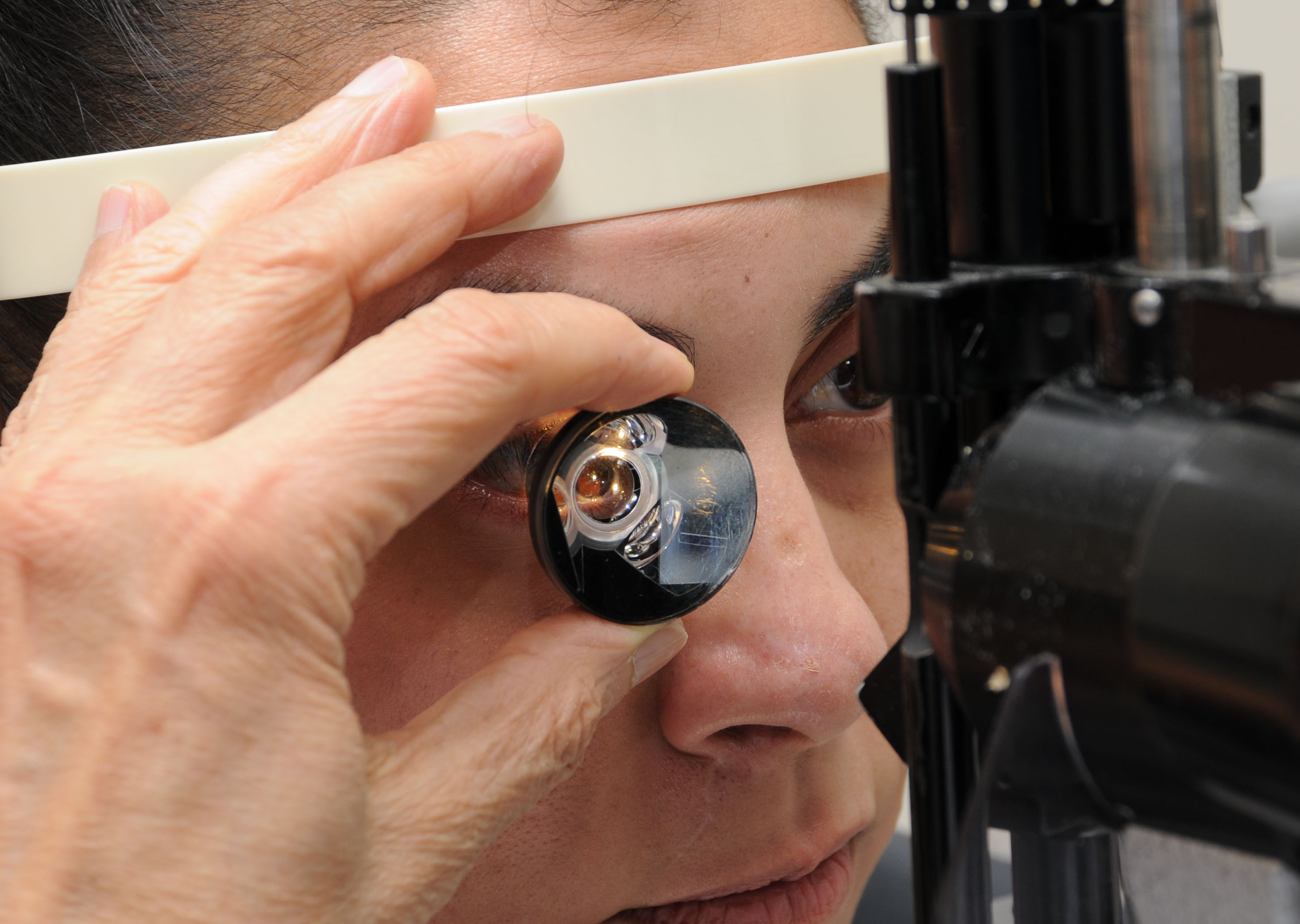 Caption: Gonioscopic exam. Source: Courtesy Karanjit Kooner MD and William Anderson, photographer, University of Texas Southwestern Medical Center, Dallas.
Because an anesthetic drop is administered before the test, gonioscopy is usually painless, although some people experience some discomfort.
Caption: Gonioscopic exam. Source: Courtesy Karanjit Kooner MD and William Anderson, photographer, University of Texas Southwestern Medical Center, Dallas.
Because an anesthetic drop is administered before the test, gonioscopy is usually painless, although some people experience some discomfort.
Beyond the Gonioscope
New technologies for examining the angle are becoming available. Anterior segment optical coherence tomography (ASOCT), which requires no anesthesia and is painless, records an image of the cross-section of the angle using a dim light reflected from the eye.After Your Gonioscopy
In most cases, an examiner can determine whether angle closure is likely, although there are instances where the results are inconclusive. Not all eye examinations include gonioscopy, but if you are considered a glaucoma suspect, you can request that your angles be examined. If there aren’t any signs or suspicion of glaucoma, the test may be considered unnecessary, but you can still ask your examiner to perform the test in order to determine if you have an anatomically narrow angle, which would put you at greater risk and indicate that periodic gonioscopy is advisable.Your History and Risk for Glaucoma
Your doctor will want to know if you have risk factors that increase the likelihood of your developing glaucoma.“How’s your vision these days?”
Clinicians often assume that the tests they perform provide all the information they need about your vision. This is not necessarily true! Don’t hesitate to let your doctor know of problems you notice. While it’s true you may not notice peripheral field loss, sometimes you do without realizing it. When you start to think about it, you might be aware of problems you hadn’t paid attention to. “Oh yes, I didn’t see that car coming in from the right at the intersection.” Dr. Jeffrey Liebman, a well-known glaucoma specialist, suggests that doctors may need a high priority checklist to ensure a comprehensive exam. Tell your doctor if you’re having trouble reading or if things looked washed out—don’t assume that these symptoms are not glaucoma simply because the doctor didn’t ask about them. You can even ask for a reading test and/or a contrast sensitivity test. Loss of contrast sensitivity is a common effect of glaucoma affecting central vision.Assessing your Results: Do you Have Glaucoma?
Your Test Results
Your test results should answer these questions for you and the doctor making a diagnosis:- Optic nerve: Do you have visible optic nerve rim and/or nerve fiber layer damage?
- Visual fields: Do you have visual field defects or scotomas that follow a glaucomatous pattern?
- Pressure: Is your IOP normal or above normal?
- Angle: Are your angles open, narrow, or closed?
- Risk factors: How many risk factors do you have?
- Corneal thickness: What is your corneal thickness measurement?
Diagnosis
If you do not have any observable optic nerve damage and do not have elevated IOP or several risk factors, you may be considered free of glaucoma and not in need of ongoing observation. If you have matching structural optic nerve and/or nerve fiber layer damage and functional visual field defects, you will most likely be given a positive diagnosis of glaucoma and either be referred to a glaucoma specialist or ophthalmologist for further evaluation or started on a glaucoma therapy. A positive diagnosis indicates the doctor believes that your present condition will worsen without treatment. Something to keep in mind is that with glaucoma, observable functional loss often follows structural loss. Although criteria for diagnosing glaucoma usually include observable and measurable structural and functional damage, optic disc and retinal nerve fiber layer structural changes are often observed before visual field defects are picked up by standard perimetry. Not only do structural changes appear to precede functional changes, but it is now possible with digital imaging to detect structural retinal nerve fiber layer damage before functional visual field impairment can be measured.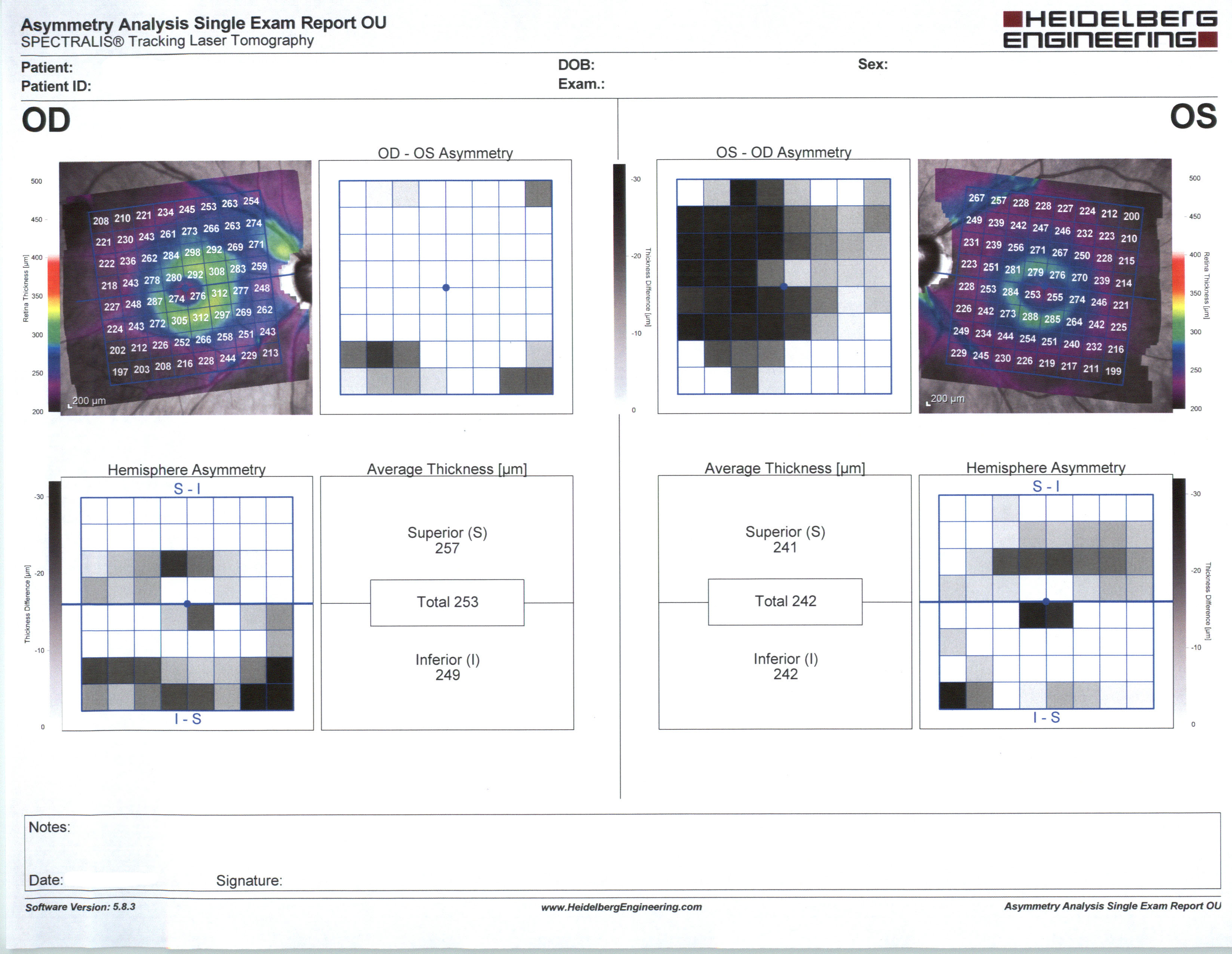 Caption: Nerve fiber scanning test in glaucoma asymmetry analysis. Source: Courtesy Karanjit Kooner MD and William Anderson, photographer, University of Texas Southwestern Medical Center, Dallas.
Caption: Nerve fiber scanning test in glaucoma asymmetry analysis. Source: Courtesy Karanjit Kooner MD and William Anderson, photographer, University of Texas Southwestern Medical Center, Dallas.
Being a Glaucoma Suspect
Often the results of testing are not clear-cut. Suspicious signs of glaucoma often precede identifiable glaucoma, and if you are a “glaucoma suspect” your doctors may suggest early treatment.Open-Angle vs. Closed-Angle
Doctors use different protocols for the monitoring and treatment of open-angle glaucoma suspects versus closed- or narrow-angle suspects. If gonioscopy reveals that your angles obscure a view of the trabecular meshwork completely or as much as 50 percent but you do not have observable structural and functional damage, you are considered an angle closure suspect. When diagnosed early enough, angle-closure glaucoma can often be cured via a procedure called a laser iridotomy. In this discussion of being a glaucoma suspect we are assuming your angle is open, which would predict a non-surgical approach to the early stages of treatment.Scenarios for Suspecting Glaucoma
If examination does not reveal structural and functional damage, what might make a doctor identify you as a glaucoma suspect? There aren’t any hard and fast rules, although attempts are being made to quantify risk. A few examples of the many possible scenarios include the following:- Higher than “normal” IOP, no risk factors, and no visible optic nerve damage.
- Higher than “normal” IOP, several risk factors, and no visible optic nerve damage.
- “Normal” IOP, several risk factors, and no observable optic nerve damage.
- “Normal” IOP, several risk factors, and possible early optic nerve damage.
Your Risk Factors
If you have several risk factors your doctor may want to monitor you closely as a glaucoma suspect.Ocular Hypertension (OHT)
There was a time when eye pressure was a primary component of the definition of glaucoma. High IOP is not glaucoma, but it is a well-documented contributing factor. If your IOP is above 21 mmHg–the high end of the average range–you may have what is now referred to as ocular hypertension and should be treated or monitored regularly. Millions of Americans are hypertensive. Only a very small percentage of those will develop glaucoma.Making the Decision on Treatment as a Glaucoma Suspect
Note to readers: This section is not intended to provide medical or treatment advice, nor is it intended to recommend a given course of treatment. Treatment decisions should only be made after consultation with your doctors. If you are identified as a glaucoma suspect, your doctor will discuss with you whether to begin treatment to minimize the risk of glaucoma developing. Why not begin treatment immediately? Glaucoma medications are expensive to purchase, time-consuming to administer, and only effective if used daily, as prescribed. Why not wait until a more definitive diagnosis is possible? Glaucoma develops slowly and its early development often doesn’t show up in examination. By the time glaucoma is apparent to an examiner, the disease has usually been active for some time and the damage done is not reversible.Evaluating Risk
Whether to wait or to begin treatment ultimately comes down to evaluating as best as one can the risk of not beginning treatment, which is something your doctor can help you determine.The Right Decision is an Informed Decision
By being well informed about the tests and studies described in this guide, you can feel confident that your doctor’s advice is based on the information she needs to assess your actual risk. With that information you can best decide how to proceed.Ask and Understand
Sometimes a doctor will examine a patient and announce a conclusion such as, “Your optic nerve looks suspicious and your pressure is high. I’m going to start you on drops to bring the pressure down.” If you are not offered a chance to discuss your diagnosis and treatment plan, ask to do so. These are decisions that can have life-long implications. Often doctors are simply rushed and need to be made aware of your need to discuss your vision, your prognosis, and decisions about treatment.Questions for Your Doctor
If you have been identified as a glaucoma suspect, make sure you first understand your test results. You might also ask the following questions:- How high a risk do you think I have? What is that assessment based on?
- How often will we be monitoring my eyes?
- What will we be monitoring? IOP? Visual fields?
- What is my specific condition?
- What is the prognosis for keeping my sight?
- What treatment options are available?
- What treatment option(s) do you recommend and why?
- What are the pros and cons of your recommended treatment versus alternative treatments?
- How might the treatment help me? What kind of improvements might I expect and how long will it take before we know if the treatment is effective?
- Are there possible side effects?
- How often will we be monitoring my eyes?
- Can you point me to a support group?
- Could my condition and my current functional vision affect my daily life, such as my ability to drive?
- Should I get a low vision assessment?
Final Thoughts on Diagnosis
Unfortunately, at this time there is no single, definitive test for glaucoma. In order to make a diagnostic decision, your doctor must evaluate many factors in order to decide if you have glaucoma or are a glaucoma suspect. The more you understand glaucoma, the more empowered you will be to take an active role in the diagnosis.Seeing Eye to Eye: You and Your Doctor
Assess Your Experience
To assess your experience with your doctor, ask yourself the following questions: Does my doctor…: …take the time to answer my questions satisfactorily and fully? …explain glaucoma in general as well as my particular form of glaucoma? …communicate in a way that helps me feel confident that I am getting complete information about what is going on with my eyes, including current IOP, optic nerve assessment, and visual field results? …ask me if I have questions? …explain how my medication(s) act and help me set up a schedule that will work for me? …ask me if I am taking my medications regularly or am missing doses? …ask if I am having side effects with my medications? …openly give her prognosis? …explain the tests she is ordering? …explain the results of my tests? …explain why she is recommending the course of treatment chosen? …invite a discussion of the pros and cons of various treatment options? …encourage me to learn more about glaucoma through books or websites such as VisionAware? …explain the importance of adhering to my treatment plan and the risks if I deviate from the plan? …have a style and personality that I am comfortable with and trust? …ask about my vision and how vision loss is affecting my daily living? …refer me to low vision services?Take Charge of the Doctor-Patient Relationship
It’s as much up to you, the patient, as it is up to your doctor to establish a mutually respectful, mature relationship. Many patients are unhappy with their experiences in treatment for glaucoma, and may suffer silently. You do not need to accept an unsatisfactory situation. First, remember that you choose your doctor. Your doctor doesn’t choose you. You can make appointments with several doctors and get a feel for different styles and approaches. How you feel about your doctor is important. If you do not feel comfortable with or trust your doctor, you may well be more likely to skip appointments and to not adhere to your medication regimen. Do you want to put your vision at risk simply because you don’t like your doctor? If you answered “No” to some or many of the questions about your doctor above, you can try to change the dynamic. Does your doctor ask if you have questions? If not, do you simply remain frustrated? You can try to shape the interaction. You can ask directly: “I have a bunch of questions. Can you spend some time during this appointment answering them?” Does your doctor explain the tests he or she performs? If not, you can ask: “Can I see the visual fields from today? How do they compare with the last tests?” Many doctors take ongoing photographic images but never show them to the patient. You can ask: “Can I see the images? Can you explain what you’re seeing? How have things changed from the previous images?”Your Medical Records
You have the right to have copies of your medical records. Few patients ask for their own copies. But you can! You can keep a file of your records and test results. You can learn a lot just by reading the doctor’s notes. They will surely raise questions for you to ask. And when your doctor knows you are keeping and looking at your records she may be more inclined to share information with you.Take Notes
Glaucoma appointments are stressful. They happen quickly, and most patients are nervous. Dealing with a disease that can take your vision can be frightening. In the midst of a rapid stressful appointment it’s easy to forget the questions you wanted to ask. Write down your questions beforehand. (If vision loss makes writing difficult for you, here are some alternative ways to record questions and answers.) It’s also easy to forget what was said in such a fast-paced, emotionally charged situation. You may get your questions answered only to find when you get home that you can’t remember what the answers were! Take notes or bring along a friend or partner who can record the session, which will free you to listen attentively. It’s very easy to forget your doctor’s instructions. Instructions are important—don’t leave them to chance. Write down any instructions your doctor gives you. And if you don’t understand the instructions, don’t just write down what you don’t understand—ask questions until you understand.Your Vision is Your Responsibility
In the end, it’s your responsibility to make sure you are in a doctor-patient relationship that works for you. This is not simply a matter of feeling good. Glaucoma is a chronic disease, so you may be with your doctor for many years. Trusting your doctor’s opinion and trusting that your doctor is listening to you will affect whether you do your part in the treatment process.Glaucoma and Your Vision
If you have glaucoma or are a glaucoma suspect who has elected to pursue treatment, you begin treatment with an ophthalmologist to treat your eye disorder and to minimize impairment to your vision. Your doctor’s focus is on changes to the anatomical and structural integrity of the eye (the drainage system, the optic nerve, and the retinal ganglion cells) and on measuring how structural changes affect the health of the organ (e.g., visual acuity and visual field). While you, the patient, certainly care deeply about these factors, you are also concerned with how you are seeing and how your vision is changing–in other words, your functional vision. With limited time to spend with each patient, the doctor’s focus is on visual health. But measuring the health of your eyes does not necessarily tell you how you are functioning. The information in this section can help you understand changes to your vision and guide you toward help for learning to adapt to your vision loss.Understanding your Vision Loss
Functional Vision
Functional vision is the use of vision for particular purposes. Functional visual skills are required to carry out everyday activities. The vision tests that are part of your glaucoma treatment may not necessarily tell that much about how you use your vision. You may measure poorly on visual field testing yet be doing fine with your daily activities. Or you may do well reading the letter chart and your visual field tests may show only moderate problems with peripheral vision, yet you experience significant visual limitations in daily living. Vision tests, while essential to the treatment of your glaucoma, may not reflect your actual experience of seeing. Functional vision is an experience that cannot be entirely measured by quantitative tests. Evaluating your experience seeing can tell you a lot about your vision. Consider the following questions.Overall Vision
- Have you noticed a change in your vision?
- Do you accomplish less than you would like because of your vision?
- Do you have difficulty reading ordinary print such as magazines or books?
- Do you have trouble finding something on a crowded shelf?
- Do you have difficulty reading traffic signs?
- Do you have trouble going down steps, stairs, or curbs in dim light or at night?
- While walking, do you have trouble noticing objects off to the side?
- Do you have difficulty seeing how people react to things you say?
- Do you have difficulty picking out and matching your own clothes?
- Do you avoid visiting with people because of your vision?
- Do you have difficulty recognizing faces, even of friends and family?
- Do you have trouble grocery shopping? Making phone calls? Taking medications?
- Can you write checks and manage other financial tasks?
- Do you have trouble driving at night? If so, what is difficult about it?
Loss of Visual Function
- Are there any blurred or distorted areas in your vision?
- Do you see lights doubled?
- Are you affected by glare outdoors, indoors, or both?
- Do you have difficulty seeing under certain lighting conditions?
- Do you notice difficulty seeing objects in low-contrast situations such as a beige sweater on a white bedspread, or figures in dark clothing by the side of the road at dusk?
- Do you see an object more clearly when you look slightly away from it?
- Do you have difficulty seeing things on the periphery of your visual field?
Restricted Visual Felds
- Do you have difficulty getting around by yourself?
- Do you have difficulty finding objects?
- Do you have difficulty functioning in poor light?
Glaucoma and Vision Loss
Vision loss from glaucoma is commonly presented as a gradual reduction in the peripheral field of vision, described and presented visually as increased tunnel vision: While narrowing of peripheral or side vision is indeed a primary characteristic of glaucoma, there are other, less frequently discussed ways glaucoma affects vision, including:- loss of contrast
- defects within the field of vision, such as distortion or blind spots
- sensitivity to glare or light
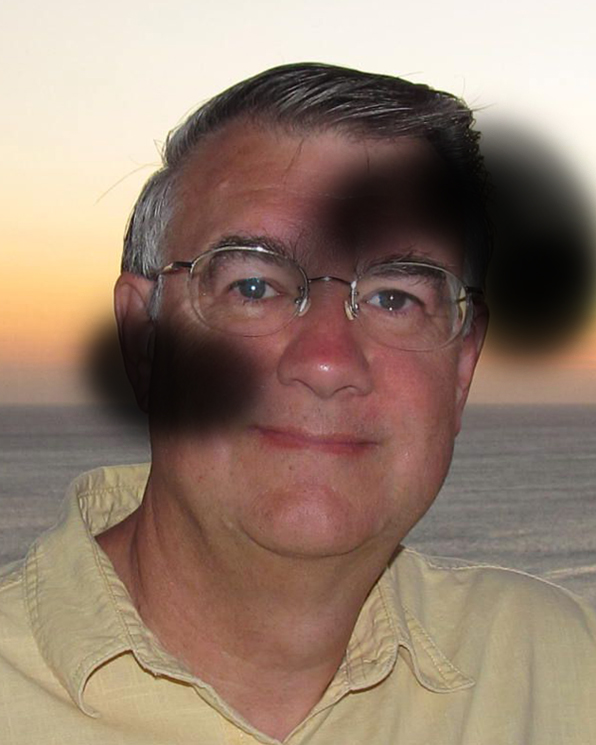 Caption: Vision distortion from glaucoma blind spots. Source: Courtesy Karanjit Kooner MD and William Anderson, photographer, University of Texas Southwestern Medical Center, Dallas.
Caption: Vision distortion from glaucoma blind spots. Source: Courtesy Karanjit Kooner MD and William Anderson, photographer, University of Texas Southwestern Medical Center, Dallas.
Contrast Sensitivity
If you have been told something along the lines of, “Your vision is good, 20/25,” but you feel that you don’t see well any more, contrast sensitivity may be the problem. Contrast sensitivity is the ability of your visual system to distinguish between an object and its background. Try picturing black beans on a white plate (high contrast) and white rice on a white plate (low contrast). Visual acuity tests present you with black letters on a white background, while in daily life most of what we see is viewed under moderate- or low-contrast conditions. If you have low contrast sensitivity, objects must have higher than normal contrast just to be visible to you. Low contrast objects and objects in low lighting situations will be difficult for you to detect. When the contrast isn’t there, everything will seem like it blends together. Caption: Stairs with high contrast (L) and stairs with low contrast (R). Source: Author.
Caption: Stairs with high contrast (L) and stairs with low contrast (R). Source: Author.
These questions can help you determine if contrast sensitivity is a problem:
Although contrast sensitivity is a very important part of functional vision, you may find your doctor doesn’t test for or even discuss it during your appointments. It may be that in a busy, rushed practice there is no time for a test that does not have diagnostic significance.
While contrast sensitivity has enormous functional significance, it is often missed.
There are tests for contrast sensitivity. Many are similar to the visual acuity test but the letters are presented in increasingly lower contrast:
- Do you have trouble driving at night? At dusk?
- Do you have trouble reading text on a computer screen?
- Do you have difficulty telling the difference between different denominations of paper money?
- Do you trip on curbs, steps, and stairs?
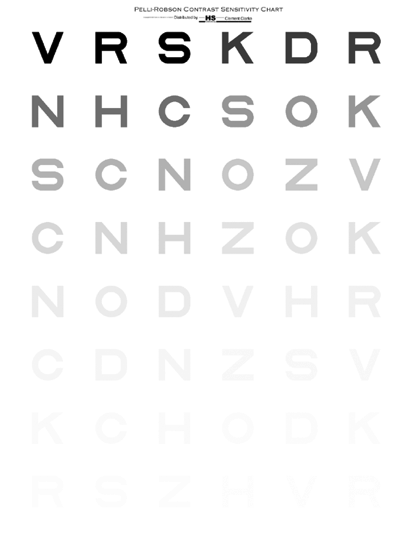 Caption: The Pelli Robson contrast sensitivity test. Source: Pelli, D. G., Robson, J. G., & Wilkins, A. J. (1988). The design of a new letter chart for measuring contrast sensitivity. Clinical Vision Sciences, 2(3):187-199. Copyright © 2014 D.G. Pelli and J.G. Robson. Manufactured by Precision Vision.
If you are concerned that your contrast sensitivity has become diminished, ask your doctor to give you a contrast sensitivity test. As an added bonus, research shows that contrast sensitivity loss from glaucomatous eye damage can be seen even before acuity loss, cupping, or field loss presents.
Caption: The Pelli Robson contrast sensitivity test. Source: Pelli, D. G., Robson, J. G., & Wilkins, A. J. (1988). The design of a new letter chart for measuring contrast sensitivity. Clinical Vision Sciences, 2(3):187-199. Copyright © 2014 D.G. Pelli and J.G. Robson. Manufactured by Precision Vision.
If you are concerned that your contrast sensitivity has become diminished, ask your doctor to give you a contrast sensitivity test. As an added bonus, research shows that contrast sensitivity loss from glaucomatous eye damage can be seen even before acuity loss, cupping, or field loss presents.
Field of Vision Defects
The tunnel model of vision loss from glaucoma is also misleading because it does not represent the more common experience of blind spots or areas of distortion that those with glaucoma often experience. These areas of defect are known as scotomas. Studies have found that patients with glaucoma report either blurring or missing areas in their peripheral fields more often than they report tunneling of their vision. Caption: A depiction of a scotoma obscuring part of a visual field. Source: National Eye Institute (image digitally altered by the author).
A scotoma may be an area of darkness—of no vision—but it may also be an area of brightness or distortion.
Caption: A depiction of a scotoma obscuring part of a visual field. Source: National Eye Institute (image digitally altered by the author).
A scotoma may be an area of darkness—of no vision—but it may also be an area of brightness or distortion.
 Caption: A visual field map showing scotomas (dark areas). Source: Author.
While scotomas show up clearly in visual field tests, where each eye is tested separately and without movement, they are often difficult to identify in real life for two reasons:
Caption: A visual field map showing scotomas (dark areas). Source: Author.
While scotomas show up clearly in visual field tests, where each eye is tested separately and without movement, they are often difficult to identify in real life for two reasons:
- We see with two eyes and a visual defect in one eye may be compensated for by the other eye.
- Our eyes move continuously (and without conscious control), creating a complete picture by putting together varied portions of the retinal images, so the scotoma can be difficult to notice.
Visual Acuity
It is easy to assume that if you read the letters on the letter chart at a reasonable visual acuity the rest of the visual system must be functioning equally well. In terms of functional vision, this is not at all necessarily true. If you hear that your “vision” is “20/25,” this refers only to the sharpness and clarity of central vision. Although you will likely be tested for acuity at each appointment, note the following:- Visual acuity tests are given in an artificial environment. The letters are high contrast black against white and thus easier to read than letters in everyday contexts.
- Acuity is only one aspect of vision. Your functional vision is much more complex, requiring the accurate and timely processing of information about size, shape, contrast, color, and motion.
- Central vision is usually the last area of vision to be affected by glaucoma.
Living with Vision Loss
Low Vision
The term “low vision” refers to a visual impairment not correctable by standard glasses, contact lenses, medicine, or surgery, that interferes with a person’s ability to perform everyday activities such as reading, driving, shopping, cooking, or watching TV. Low vision manifests in many ways. You may have severely reduced visual acuity, a significantly obstructed field of vision, or reduced contrast sensitivity—or all three! You may not actually know you have low vision! People often struggle in their daily life without understanding why. To make best use of your vision, you need to become aware of several factors, including the following:- Your near and far visual acuity.
- Whether your visual field is full or restricted.
- The effects of light and glare on your vision.
- Your ability to recognize colors.
- How loss of contrast sensitivity affects your visual functioning.
- How you are able to use vision for particular purposes.
Improving Functional Vision
Do you have trouble reading, driving, or walking in dimly lit spaces or streets? Loss of contrast sensitivity can make these tasks challenging. Glare—light coming into your eye from the top or side—can also make seeing difficult. Contrast sensitivity and glare tests can be performed as part of your low vision assessment. Do you have difficulty driving? If you have glaucoma, can you realistically assess your driving? How can you know what you don’t see? Even when treatment cannot reverse vision loss, functional vision—how you function in the world—may be improved with training and with vision-enhancing devices. You can learn to make better use of your vision and you can function efficiently with only small amounts of visual information. The first step in adapting to the vision loss you are experiencing from glaucoma is to make an appointment with a low vision specialist who will help you recognize and accept the ways glaucoma has affected your vision and help you learn new strategies for functioning independently. Visit VisionAware to learn more about low vision exams and living with vision loss. You may also want to try our Getting Started Kit for more tips and ideas.The Future of Glaucoma Research and Treatment
Researchers are pursuing many new avenues to investigate the underlying causes of glaucoma. As researchers learn more about the disease process involved with glaucoma, new diagnostic and treatment processes are being developed and studied. You may want to read about existing treatments. But exciting new areas of investigation include the following:- New imaging technologies for diagnosing and tracking glaucoma.
- New treatments for those with glaucoma:
- Neuroprotection
- New medications
- Laser research
- New surgical procedures
- Research into the genetics and cell biology that underlie glaucoma.
- Preventive therapies.
- New ways of thinking about glaucoma.
Diagnostic Imaging
New techniques for seeing and creating images of the optic nerve and retinal nerve fiber layer are continually evolving, and currently include: Confocal scanning microscopy, Fourier-Domain optical coherence tomography, multifocal visual-evoked potentials, microperimetry, and retinal functional imaging, along with Spectralis analysis and improving imaging of retinal ganglion cells.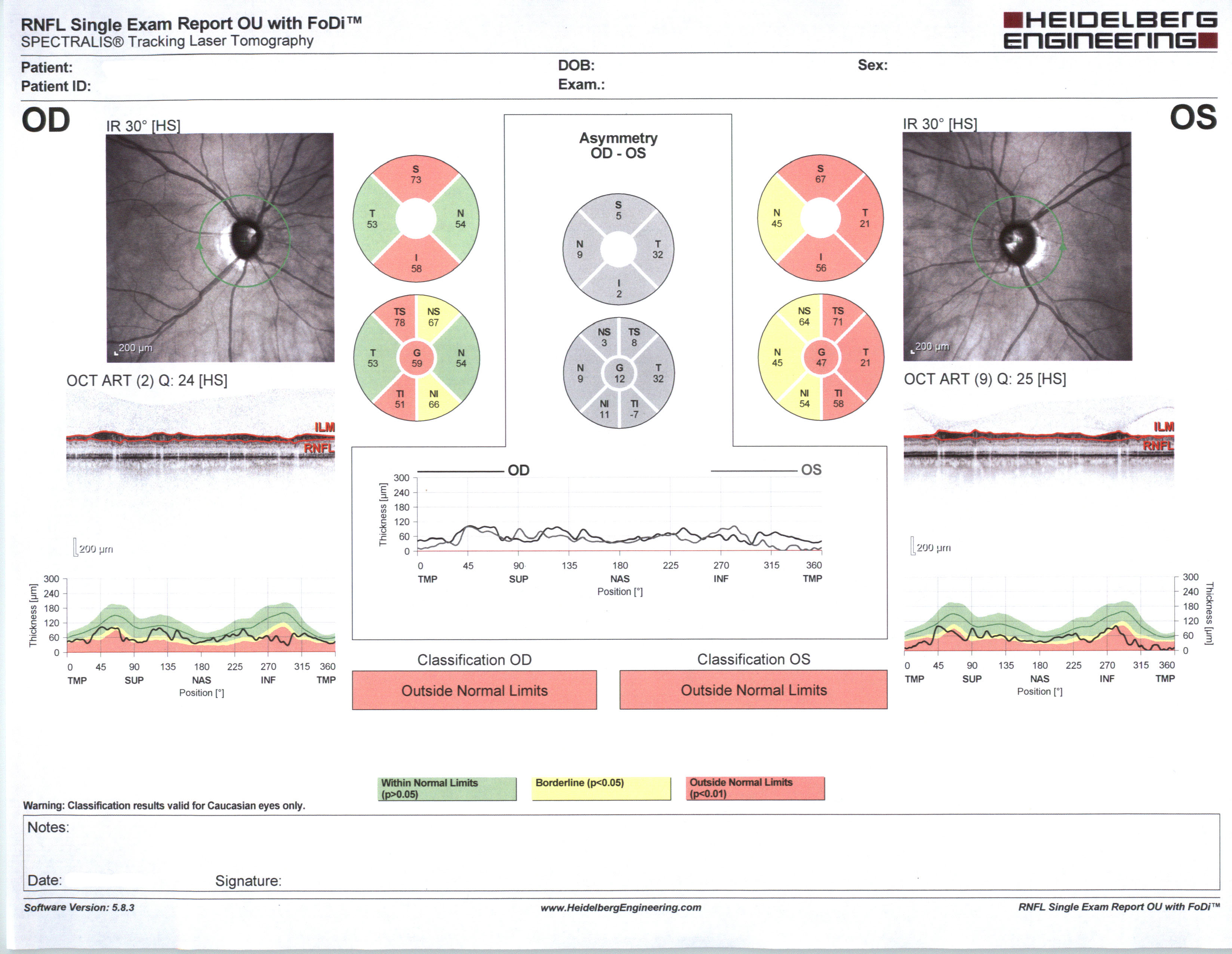 Caption: Nerve fiber layer analysis in glaucoma. Source: Courtesy Karanjit Kooner MD and William Anderson, photographer, University of Texas Southwestern Medical Center, Dallas.
Caption: Nerve fiber layer analysis in glaucoma. Source: Courtesy Karanjit Kooner MD and William Anderson, photographer, University of Texas Southwestern Medical Center, Dallas.
New Treatments
Neuroprotection Research
Controlling the progression of glaucoma has until recently focused on the lowering of IOP. Because glaucoma does progress in some individuals despite good control of pressure, research into medicines that strengthen the eye against the effects of high pressure (neuroprotective agents) is one of the most promising areas of investigation. Neuroprotection as a strategy for glaucoma treatment aims to employ agents that will prevent or delay retinal ganglion cell (RGC) death and will save and promote regeneration of already compromised RGCs. Neuroprotection research seeks to identify agents that can:- Protect neurons before the onset of a destructive influence.
- Rescue neurons already compromised.
- Promote the regrowth of neurons’ axons and dendrites, restoring connections that can lead to restored function.
- Researchers have found pathways that lead to ganglion cell death as well as survival pathways that keep the nerve cells alive, which are activated at the onset of an injury. The goal now is to learn how to block the death pathways and/or strengthen the survival pathways.
- RNA (ribonucleic acid), the molecule that carries out the genetic code, may be enlisted to interfere with the activity of a mutant gene that threatens neurons or axons.
Drug Studies
Development and evaluation of new medicines that lower intraocular pressure or increase fluid outflow is ongoing. Examples include:- A medication that would loosen the connection between the cells of the trabecular meshwork, potentially allowing debris clogging the meshwork to be released.
- An alternative to daily eye drops delivered by injection under the conjunctiva near the cornea in a slowly biodegradable form, potentially providing pressure reduction for up to 3–6 months.
Laser Research
- The titanium-sapphire laser for the treatment of open-angle glaucoma has recently received FDA approval.
Surgical Procedures
Until recently, surgery was considered as a last resort for open-angle glaucoma treatment, only after medication failed to control IOP. The complications associated with trabeculectomy, the surgical procedure used to treat open-angle glaucoma, kept it from being a popular first choice. With the advent of new surgical techniques and technology, this balance may well be changing. New surgical interventions now available or under investigation include: Other new surgical interventions include canaloplasty to widen the Schlemm’s canal; the gold shunt implant; ologen gel, a microtechnology-based, biodegradable membrane; and minimally invasive Trabectome surgery. You can read more about these interventions at New York Glaucoma Research Institute.The Genetics of Glaucoma
By comparing the genetic makeup—or genome—of people who have glaucoma to people who are free from glaucoma, researchers are attempting to identify the genetic differences that put people at risk for glaucoma. The effort is complicated by the fact that glaucoma seems to be influenced by many small genetic differences rather than a single gene. Five regions of the genome have been found to be strongly associated with open-angle glaucoma, with certain genes associated with eye pressure and others associated with the optic nerve. At least two of the genes linked to higher eye pressure are thought to affect the trabecular network and hence fluid flow.The Candidate Gene
In the candidate gene approach, researchers make a list of candidate genes that might cause glaucoma if their normal function were altered and then test a large group of unrelated glaucoma patients for defects in these candidate genes. Candidate genes having functions that may be important in glaucoma include the following:- Genes active in the drainage angle where fluid exits the eye.
- Genes active in the ciliary body where fluid enters the eye.
- Genes with functions that suggest they regulate the intraocular pressure.
- Genes that may be important in maintaining the health of the optic nerve.
Linkage Analysis
In the linkage analysis approach to genetic causes, glaucoma-causing genes are identified by studying large families that have several members with glaucoma. Those segments of the DNA always passed down through the family along with glaucoma are located within linked regions of DNA.Modifier Genes
Researchers are “investigating the presence of modifier genes in various glaucomas and correlating these with the age of onset and severity of the glaucoma.” Modifier gene studies include:- Seeking to identify genes that can be manipulated to increase retinal ganglion cell (RGC) (the output nerve cells of the retina) survival, which are critical because RGCs connect the eye to the brain.
- Identifying the molecules and genes that are activated in sick RGCs, ultimately providing “an integrated understanding of RGC death in glaucoma that will identify key targets for genetic therapy.”
Glaucoma and the Brain
Because glaucoma continues to progress in some patients who have successfully lowered their pressure, other factors in disease progression are being explored. Research has shown that glaucomatous nerve damage in the eye may spread to major visual centers of the brain (a process well known in other neurodegenerative diseases). When the damage spreads, nerve cells in the brain related to visual function begin to shrink and die. Neuroprotection has the potential to prevent the degeneration of those nerve cells both in the eye and the brain itself. A 2006 study showed that memantine protects neurons from shrinkage in the vision centers of the brain in experimental glaucoma. Clinical trials are underway to determine if glaucoma patients will benefit.New Paradigms
Recent research suggests that cells in the retina other than RGCs are equally affected or equally contribute to the rate of decline of the ganglion cells. This suggests looking at the occurrence of neurodegeneration in a new light, with research underway to identify connections in the brain and how these connections may be strengthened.Glaucoma as a Neurologic Disorder
Many researchers no longer view glaucoma as an eye disease but rather a neurologic disorder that causes nerve cells to degenerate and die, much like in Parkinson’s and Alzheimer’s diseases. Focusing on the mechanisms that cause the degeneration of RGCs—which connect the eye to the brain through the optic nerve—researchers are seeking ways to protect, enhance, and even regenerate ganglion cells. Many treatments that target retinal ganglion cells are now in clinical trials, including:- Injecting medications into the eye to deliver survival and growth factors to ganglion cells.
- Administering medications known to be useful for stroke and Alzheimer’s, such as cytidine-5-diphosphocholine.
- Delivering electrical stimulation to RGCs via tiny electrodes implanted in contact lenses or other external devices.