Although the advent of anti-VEGF therapy (explained below), administered via eye injection with Lucentis, Eylea, or Avastin, has revolutionized the treatment of wet age-related macular degeneration (AMD), there are still a number of persons who do not respond to treatment. It is these “non-responders” or “reduced responders” who continue to pose significant challenges to doctors and researchers.
Despite the relative success of these drugs in treating (but not curing) wet AMD, retinal specialists acknowledge the need for additional interventions to treat wet AMD more effectively. One promising approach that entered several Phase 3 clinical trials earlier this year explored the treatment of wet AMD by inhibiting both vascular endothelial growth factor (VEGF) and platelet-derived growth factor (called PDGF, also explained below), via the injectable drug Fovista, a new drug candidate from Ophthotech.
Unfortunately, although this innovative approach showed promise, Fovista did not prove to be effective when data from two of the drug’s Phase 3 clinical trials – during which it was administered in combination with Lucentis – was analyzed.
The Clinical Trial Results
On December 12, 2016, Ophthotech released the following information (edited for length and clarity):
Ophthotech Corporation today announced that the pre-specified primary endpoint [i.e., indicator of success] of mean [or average] change in visual acuity at 12 months was not achieved in its two pivotal Phase 3 clinical trials investigating the superiority of Fovista® … anti-PDGF therapy in combination with Lucentis® … anti-VEGF therapy compared to Lucentis® monotherapy [i.e., using Lucentis alone] for the treatment of wet age-related macular degeneration (AMD). The addition of Fovista® to a monthly Lucentis® regimen did not result in benefit as measured by the mean change in visual acuity at the 12 month time point.
“We are very disappointed in the results from these trials, particularly for patients afflicted with wet AMD,” commented David R. Guyer, M.D., Chief Executive Officer of Ophthotech. “We are thankful to the patients and clinical investigators and their staff for participating in the trials. We will continue to analyze the data from these two studies to better understand the trial results.”
The two clinical trials (OPH1002 and OPH1003) were international, multicenter, randomized, double-masked, controlled Phase 3 studies evaluating the safety and efficacy of 1.5 mg of Fovista® administered in combination with Lucentis® (called Fovista® combination therapy) compared to Lucentis® monotherapy [i.e., Lucentis alone]. In each of these trials, patients were randomized to one of two approximately equal-sized treatment groups. The two Phase 3 trials enrolled … 1,248 patients with wet AMD.
To better understand these results, it is helpful to understand the processes that underlie wet AMD, along with its current treatments (but not cures).
What is Wet Age-Related Macular Degeneration (AMD)?

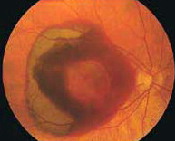
In wet macular degeneration, the choroid (a part of the eye containing blood vessels that nourish the retina) begins to sprout abnormal blood vessels that develop into a cluster under the macula, called choroidal neovascularization (neo = new; vascular = blood vessels).
The macula is the part of the retina that provides the clearest central vision. Because these new blood vessels are abnormal, they tend to break, bleed, and leak fluid under the macula, causing it to lift up and pull away from its base. This damages the fragile photoreceptor cells, which sense and receive light, resulting in a rapid and severe loss of central vision.
What Is Angiogenesis?
Angiogenesis is a term used to describe the growth of new blood vessels and plays a crucial role in the normal development of body organs and tissue. Sometimes, however, excessive and abnormal blood vessel development can occur in diseases such as cancer (tumor growth) and AMD (retinal and macular bleeding).
Substances that stop the growth of these excessive blood vessels are called anti-angiogenic (anti=against; angio=vessel; genic=development), and anti-neovascular (anti=against; neo=new; vascular=blood vessels).
Angiogenesis and Anti-VEGF Treatments
The focus of current anti-angiogenic drug treatments for wet AMD is to reduce the level of a particular protein, called vascular endothelial growth factor, or VEGF, that binds to cells on the inner lining of blood vessels (vascular endothelial cells) and promotes their abnormal growth in the retina and macula; thus, these drugs are classified as anti-VEGF treatments. At present, these drugs (Lucentis, Eylea, or Avastin) are administered by injection with a very small needle directly into the eye after the surface has been numbed.
A New Approach: Angiogenesis and Anti-PDGF Treatments
In contrast with vascular endothelial growth factor (VEGF), which binds to cells on the inner lining of blood vessels (endothelial cells), platelet-derived growth factor (PDGF) binds to cells on the outer lining of blood vessels (pericytic cells or pericytes).
Thus, VEGF and PDGF play related, but separate, roles in the formation and growth of new blood vessels: While VEGF stimulates abnormal blood vessel growth in the retina and macula, PDGF stabilizes the maturing blood vessels and shields the inner/endothelial cells, keeping them alive despite anti-VEGF treatment. The result? The Lucentis, Eylea, or Avastin treatment can be rendered ineffective, as seen in persons who are “non-responders” and “reduced responders.”
Researchers theorize, therefore, that a combined anti-VEGF and anti-PDGF treatment, targeting both immature and maturing blood vessels, may be more effective than anti-VEGF treatment alone (called “monotherapy”). The anti-PDGF therapy strips the pericytic/protective cells from the outer blood vessel coverings; when the outer protective cells are gone and the inner endothelial cells are exposed, the anti-VEGF therapy can eliminate them as well.
Current Research: Anti-PDGF Treatments
Fovista
Fovista is an anti-PDGF drug candidate from Ophthotech for the potential treatment of wet AMD, used in combination with anti-VEGF drugs. Ophthotech is a United States-based biopharmaceutical company that “specializes in the development of novel therapeutics to treat diseases of the back of the eye, with a focus on developing therapeutics for age-related macular degeneration.” Since Fovista is injected into the eye via a separate needle from the anti-VEGF drug, treatment requires two separate injections.
Please note: Although the unsuccessful clinical trial reported here involved Fovista combined with the anti-VEGF drug Lucentis, simultaneous clinical trials have been in progress with the anti-VEGF drugs Avastin and Eylea. Results from those clinical trials have yet to be released.
The Durasert Insert from pSivida
Another anti-PDGF treatment in development is the Durasert Sustained-Release Insert from the biotechnology company pSivida. The company has also developed the FDA-approved injectable implant ILUVIEN, in a partnership with Alimera Sciences, for the treatment of diabetic macular edema.
The sustained-release insert is designed to deliver a repurposed cancer drug, called TKI, which is known to block the action of both VEGF and PDGF. Thus far, the insert has been used only in two pre-clinical animal studies. According to pSivida, the ultimate goal of the Durasert project is to “effectively treat AMD on a sustained basis for six months with a single injection, targeting both VEGF and PDGF while avoiding the toxic systemic side effects of [cancer drugs] and the frequent injections of current AMD anti-VEGF [injections].”
About Clinical Trials
Most clinical trials are designated as Phase 1, 2, or 3, based on the questions the study is seeking to answer:
- In Phase 1 clinical trials, researchers test a new drug or treatment in a small group of people for the first time to evaluate its safety, determine a safe and effective dosage range, and identify possible side effects.
- In Phase 2 clinical trials, the study drug or treatment is given to a larger group of people to determine if it is effective and to further evaluate its safety.
- In Phase 3 studies, the study drug or treatment is given to even larger groups of people (1,000-3,000) to confirm its effectiveness, monitor side effects, compare it to commonly used treatments, and collect information that will allow the drug or treatment to be used safely.
- In Phase 4 studies, after the United States Food and Drug Administration (FDA) has approved the drug, continuing studies will determine additional information, such as the drug’s risks, side effects, benefits, and optimal use.
VisionAware will provide updates on this macular degeneration research as they become available.