
New glaucoma research from the University of Michigan indicates that patterns of adherence to glaucoma medication regimens, both positive and negative, that are established during the first year tend to persist over time.
According to the research team, these results suggest that “investing resources in both identifying and helping patients with [less than optimal] adherence patterns over the first year may have a large impact on longer-term adherence.”
“If we can increase people’s contact with the healthcare system in new ways — it doesn’t necessarily have to be with the doctor, it could be a health educator — we could impact the disease,” says [study author] Dr. Paula Newman-Casey, who also suggests that effective glaucoma care should consider following a more intensive and supportive model, such as that used in diabetes care, which uses community-based diabetes educators as a critical component of the multi-disciplinary diabetes healthcare team.
Ophthalmology: the Journal
The research, entitled Patterns of Glaucoma Medication Adherence over Four Years of Follow-Up, has been published online ahead of print in the August 24, 2015 edition of Ophthalmology, the official journal of the American Academy of Ophthalmology.
Ophthalmology publishes original, peer-reviewed research in ophthalmology, including new diagnostic and surgical techniques, the latest drug findings, and results of clinical trials. The authors are Paula Anne Newman-Casey, Taylor Blachley, Paul P. Lee, Michele Heisler, Karen B. Farris, and Joshua D. Stein, from the University of Michigan, Ann Arbor Medical School, College of Pharmacy, and Institute for Health Care Policy and Innovation.
About Open-Angle Glaucoma
Glaucoma is a group of eye diseases that damage the optic nerve and is one of the leading causes of vision loss and blindness. Open-angle glaucoma is the most common form of glaucoma.
The eye continuously produces a fluid, called the aqueous (or aqueous humor), that must drain from the eye in order to maintain healthy eye pressure. Aqueous humor is a clear, watery fluid that flows continuously into, and out of, the anterior (or front) chamber of the eye, which is the fluid-filled space between the iris and the cornea. It is the aqueous that helps to bring nutrients to the various parts of the eye.
Aqueous fluid drains from the anterior chamber through a filtering meshwork of spongy tissue along the outer edge of the iris (called the trabecular meshwork), where the iris and cornea meet, and into a series of “tubes,” called Schlemm’s canal, that drain the fluid out of the eye. Problems with the flow of aqueous fluid can lead to elevated pressure within the eye.
In primary open-angle glaucoma, the filtering meshwork may become blocked or may drain too slowly. If the aqueous fluid cannot flow out of the eye, or flow out quickly enough, pressure builds inside the eye and can rise to levels that may damage the optic nerve, resulting in vision loss.
Most eye care professionals define the range of normal intraocular [i.e., within the eye] pressure (IOP) as between 10 and 21 mm Hg [i.e., millimeters of mercury, which is a pressure measurement]. Most persons with glaucoma have an IOP measurement of greater than 21 mm Hg.
If you have been diagnosed with glaucoma, it is critical that you maintain the eye drop medication regimen prescribed by your eye doctor. In order for the medication to lower your intraocular pressure effectively, consistent daily adherence to your prescribed eye drop regimen is essential.
Vision Loss from Glaucoma
Glaucoma results in peripheral (or side) vision loss initially, and as this field loss progresses, the effect is like looking through a tube or into a narrow tunnel. This constricted “tunnel vision” effect makes it difficult to walk without bumping into objects that are off to the side, near the head, or at foot level.
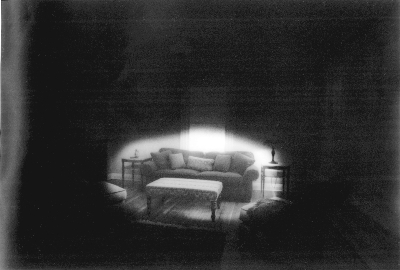
A living room viewed through a constricted visual field.
Source: Making Life More Livable. Used with permission.
Glaucoma is an especially dangerous eye condition because most people do not experience any symptoms or early warning signs at the onset. Glaucoma can be treated, but it is not curable. The damage to the optic nerve from glaucoma cannot be reversed.
About the Glaucoma Adherence Research
Excerpted/Adapted from Glaucoma Medication Reminders May Improve Adherence from Medscape Multispecialty News (registration required):
Previous studies have suggested that 30% to 80% of people with glaucoma do not take their medications as prescribed, but it is difficult for physicians to tell which patients are taking the drugs and which are not. Patients often overestimate the amount they are taking and tend to take the medications just before seeing their physicians.
To get a better idea of which patients are most likely to miss doses, [study author Dr. Paula Newman-Casey] and colleagues analyzed data from Clinformatics DataMart (pdf file), a database from a large managed care network. The database included procedures, office visits, prescriptions filled, and socio-demographics for 15,914,449 eye care beneficiaries throughout the United States.
The researchers focused on 1,234 patients who were at least 40 years old and who were newly diagnosed and treated for open-angle glaucoma. They measured adherence by dividing the number of days the patients had the correct amount of medication on hand by the number of days in the study period.
The researchers identified five patterns of adherence:
- persistently good adherence
- persistently moderate adherence
- declining adherence
- persistently very poor adherence
- never adherent
The researchers calculated patterns during the first year and patterns over the course of four years. They found that 49.7% of patients stayed in the same group for all four years.
Next, the research team analyzed the factors that correlated to the different types of adherence:
- In the one-year analysis, patients in the persistently good adherence group were more likely to be older, to be white, and to have a higher first medication co-payment cost.
- Patients in the never-adherent and declining adherence groups were more likely to report lower annual incomes (less than $60,000) and get their prescriptions from a store pharmacy instead of mail-order or both mail-order and pharmacy.
- These same characteristics were still significant in the four-year analysis.
- Those who made three visits to an eye care provider in the first year of follow-up were 1.8 times more likely to adhere than those who made fewer visits.
- Those who paid more for their prescriptions were less likely to adhere.
The Takeaway
“If we can increase people’s contact with the healthcare system in new ways — it doesn’t necessarily have to be with the doctor, it could be a health educator — we could impact the disease,” said Dr. Newman-Casey. “We could increase people’s contact with the healthcare system by embracing more team-based care, where the physician works with health educators to make sure patients really understand their disease.”
She suggested that glaucoma care might follow a model such as that used in diabetes: Both are diseases in which the patient is typically not bothered by symptoms, she pointed out. “Glaucoma is a similarly insidious condition, and we need a similar model of care,” she said.
Also, physicians could consider cost, she suggested. “Physicians should consider whether a less expensive alternative is available for their patients, like a generic medication,” she said. “Bringing up cost may be an embarrassing topic for patients, so it is important for physicians to bring it up as a possible issue.”
[Editor’s note: For more information on related glaucoma compliance research, see Can Generic Drugs Improve Compliance with Glaucoma Medication Regimens? New Research Says Yes on the VisionAware blog.]
More about the Research from Ophthalmology
From the article abstract:
Purpose: To assess longer-term patterns of glaucoma medication adherence and identify whether patterns established during the first year of medication use persist during three subsequent years of follow-up.
Participants: Beneficiaries aged 40 years [and older] who were enrolled in a United States (US)-managed care plan for seven years [or more] between 2001 and 2012 and newly diagnosed and treated for open-angle glaucoma.
Results: Of the 1,234 eligible beneficiaries, [we] identified five distinct glaucoma medication adherence patterns in both the 1-year and 4-year follow-up periods. These groups were as follows:
- Never adherent after their initial prescription fill (7.5% and 15.6% of persons in the 1- and 4-year models, respectively);
- Persistently very poor adherence (14.9% and 23.4% of persons in the 1- and 4-year models, respectively);
- Declining adherence (9.5% and 9.1% of persons in the 1- and 4-year models, respectively);
- Persistently moderate adherence (48.1% and 37.0% of persons in the 1- and 4-year models, respectively);
- Persistently good adherence (20.0% and 15.0% of persons in the 1- and 4-year models, respectively).
More than 90% of beneficiaries in the four groups with the worst and best adherence patterns (groups 1, 2, 3, 5) maintained their patterns from their first year throughout their four years of follow-up.
Persons with the best adherence over four years were more likely to be white, to be older, to earn more than $60,000/year, and to have more eye care visits. Those with a higher initial co-payment cost had lower adherence rates.
Conclusions: For most patients who were newly prescribed glaucoma medications, adherence patterns observed in the first year of treatment reflect adherence patterns over the subsequent three years. Investing resources in both identifying and helping patients with [less than optimal] adherence patterns over the first year may have a large impact on longer-term adherence.